Stomach
Polyps
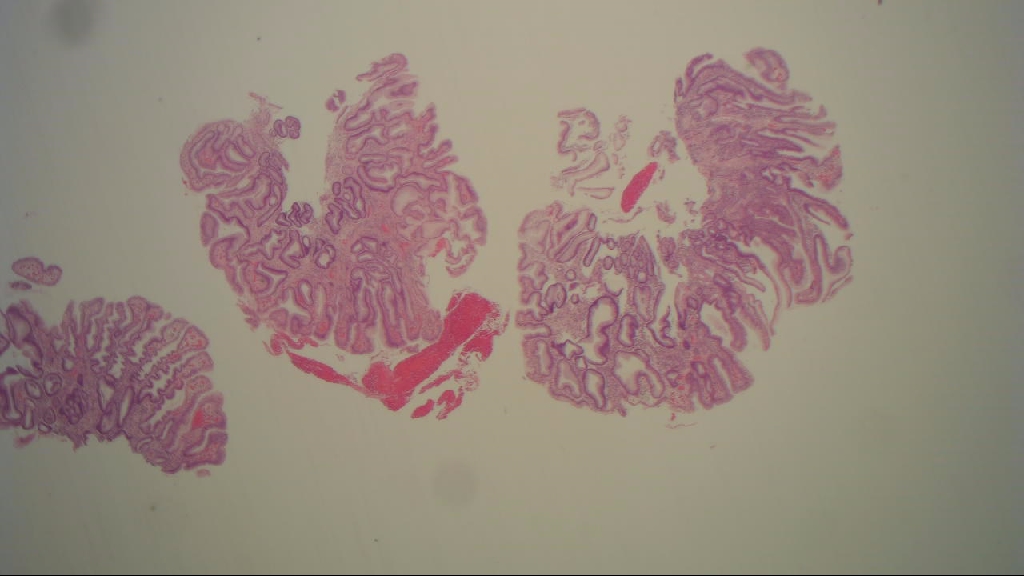
Hyperplastic polyp
Reviewers: Elliot Weisenberg, M.D. (see Reviewers page)
Revised: 8 August 2012, last major update August 2012
Copyright: (c) 2003-2012, PathologyOutlines.com, Inc.
General
=========================================================================
● Also called inflammatory, regenerative polyps
● Different from colonic hyperplastic polyps but similar to colonic inflammatory pseudopolyps
● Non-neoplastic, represents about 75% of all gastric polyps
● Associated with background mucosal disease in 85% of cases, particularly chronic gastritis with glandular atrophy and intestinal metaplasia; H. pylori gastritis, chemical (reactive) gastropathy, thus, endoscopists should also biopsy surrounding mucosa to evaluate underlying gastric abnormalities
● Also associated with hypochlorhydria and hypergastrinemia
● Multiple polyps associated with autoimmune gastritis
● Usually age 50+
● Rare/no malignant potential by itself, although present in 20% of stomachs resected for carcinoma (chronically inflamed and atrophic mucosa tends to form hyperplastic polyps and to degenerate into malignancy)
● Hyperplastic polyps with even low grade dysplasia may have significant risk for associated carcinoma (Hum Pathol 2002;33:1016)
Gross description
=========================================================================
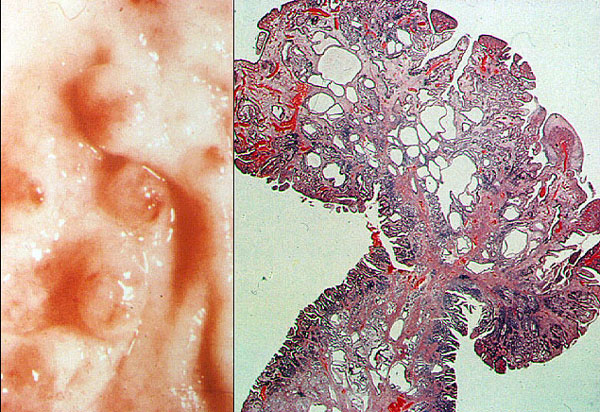
● Small (mean 1.4 cm, range 0.5 to 2 cm), sessile, multiple (20%), 60% in antrum
● Smooth or slightly lobulated
● Central umbilication common, more proximal when associated with autoimmune gastritis
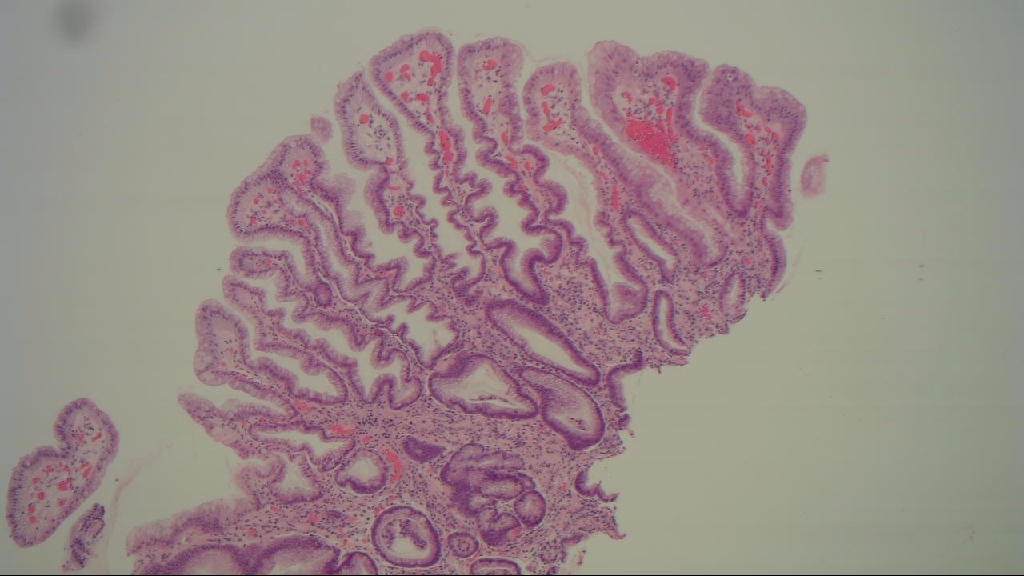
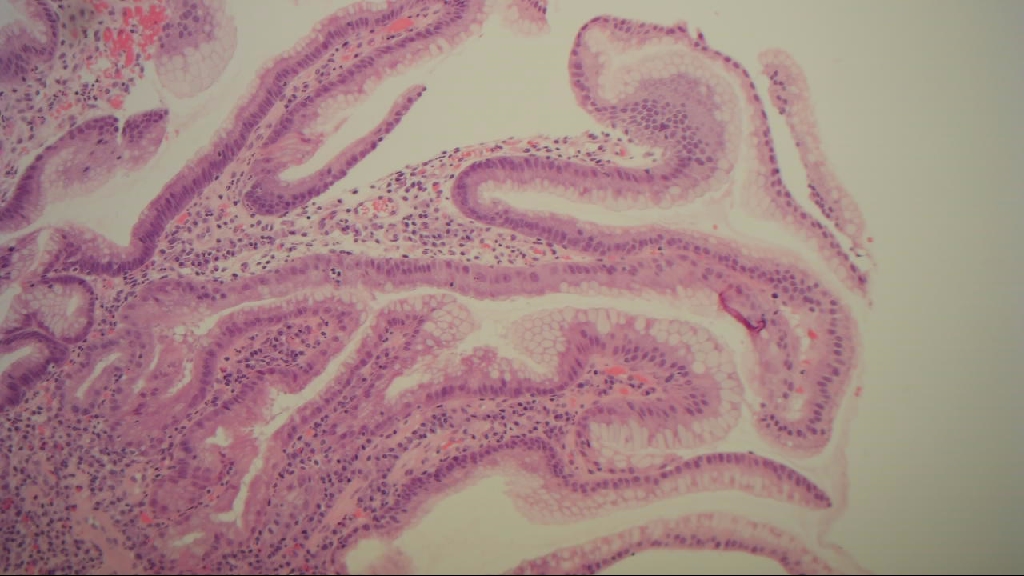
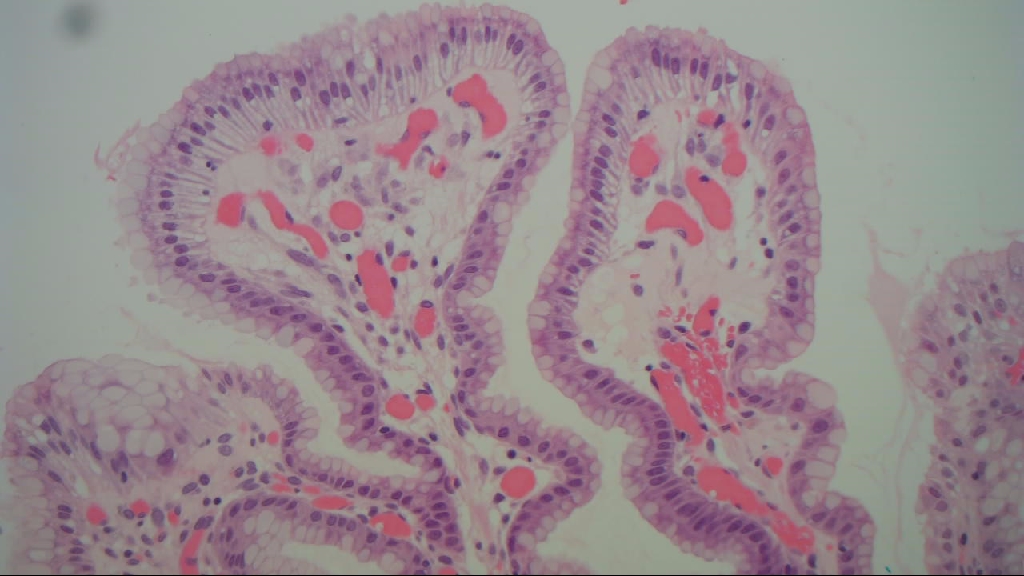
Micro description
=========================================================================
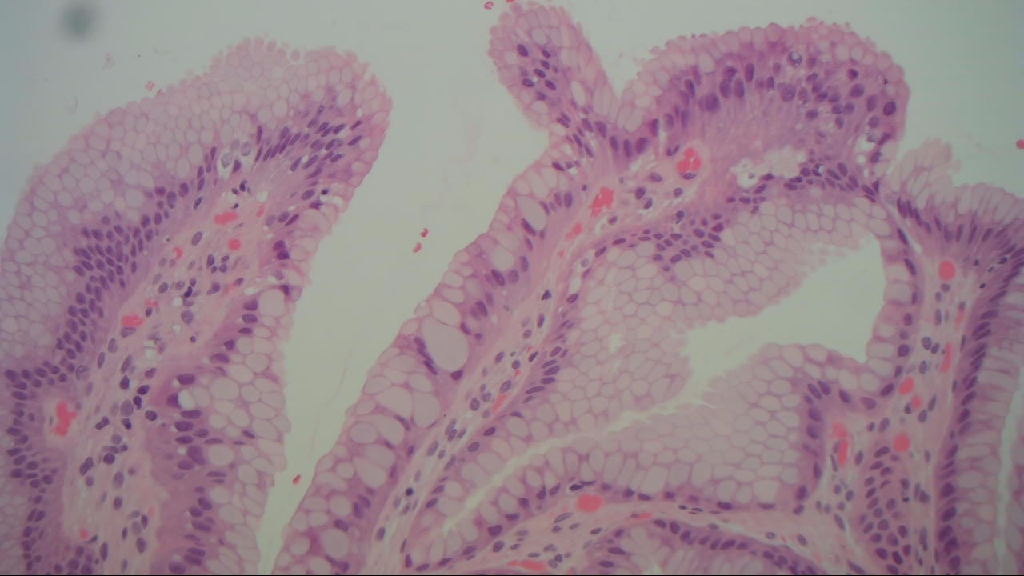
● Elongated, tortuous or dilated gastric foveola with pyloric or fundic glands (Am J Surg Pathol 2001;25:500)
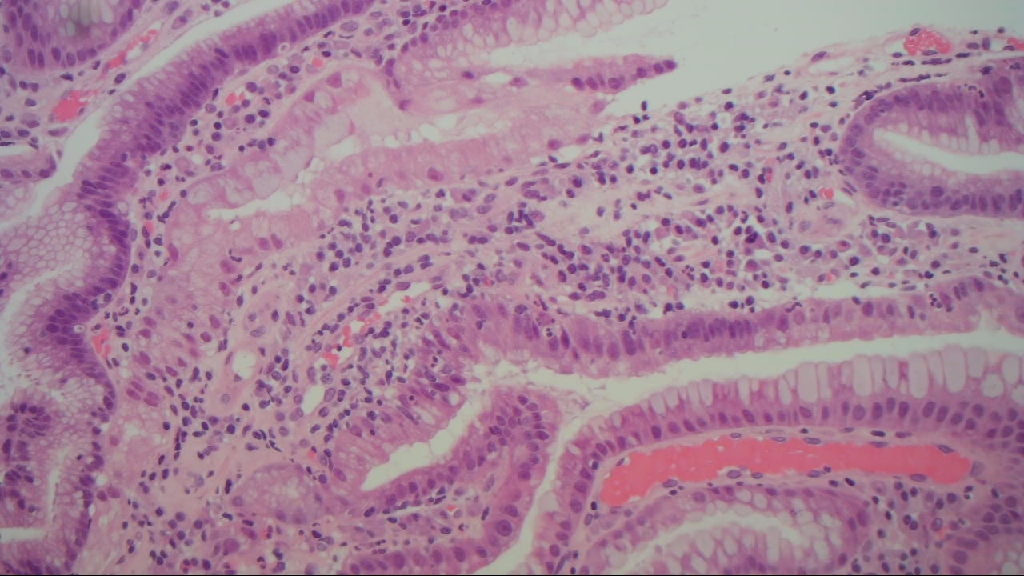
● Lamina propria has inflammatory cells, scattered smooth muscle bundles, edema, patchy necrosis
● Associated with chronic, active (H. pylori), reactive gastritis, and atrophic autoimmune gastritis
● Rarely foamy macrophages
● Surface mucosa may be regenerative, but dysplasia in only 4%
● Focal intestinal metaplasia in 16%
● May regress when H. pylori gastritis is treated
Micro images
=========================================================================